
In late 2019, we became aware of Severe Acute Respiratory Syndrome Coronavirus 2, the viral etiology of coronavirus disease 2019 (COVID-19). But it was not until late February or early March that it affected our health care system in a major way. On March 7, 2020 New York State (NYS) Governor Andrew Cuomo signed Executive Order (EO) No. 202 and declared a Disaster Emergency in NYS. On March 11, the World Health Organization declared that the COVID-19 outbreak had reached pandemic status. In a subsequent EO on March 20, dental services in NYS were limited to urgent/emergency care only. On that day the governor called upon all licensed professionals including dentists to come to the aid of their colleagues dealing with the COVID-19 pandemic. At the end of March, while the dental clinics at the Jacobi Medical Center (JMC) in the Bronx, New York were providing only emergent and urgent care, the rest of the hospital was being overwhelmed by the influx of COVID-19 patients. All vacations were cancelled and all able-bodied people were called upon to assist in the effort. The hospital’s Chief Executive Officer, Chief Medical Officer, and Chairs of the Medicine, Surgery, and Emergency departments requested help from their hospital colleagues who were not on the front lines or were not already performing urgent patient care. The situation was so dire that a call went out to the Armed Forces Medical Reserve Corps, and by April 7, 122 Air Force and Army reservists came to JMC to provide care. This is a case study of the response of a hospital-based dental practice to the Corona-19 pandemic.
Background
The Environment
Jacobi Medical Center (JMC) is located in the Bronx, a New York City borough of 1.425 million people. The U.S. Census Bureau considers the Bronx to be the most ethnically and linguistically diverse area in the country. There is an 89.7% chance that any two residents, chosen at random, would be of different race or ethnicity. The majority (55.7%) of the population speak non-English languages at home, with a recent significant rise in African languages. According to a report released in late 2015, more than 192 languages are spoken in the New York metropolitan area. In addition to its great population diversity, the Bronx boasts great historical attractions and , including the Botanical Garden, Bronx Zoo, and Yankee Stadium. Unfortunately, the borough is best known for its housing projects, vast swathes of poverty and domestic crowding, and being the least healthy county out of the 60 counties in NYS.
By the end of May, the Bronx had the highest prevalence of COVID-19 infected individuals in NYS. An even more impressive statistic considering that at that time, NYS had the highest prevalence among all U.S. states. On May 20, 38-51% of the population in the Bronx tested positive for antibodies, and the local area around JMC had among the highest hospitalization rate (5.91/100,000 people) in the US.
The Hospital
JMC is part of the municipal hospital system of the City of New York City/Health + Hospitals. It is a 450-bed, 54 mixed ICU bed, level 1 trauma center, and part of the safety net for patients who are indigent and/or underserved. The hospital system credo is to take care of patients regardless of their ability to pay. JMC is also a major teaching hospital for the Albert Einstein College of Medicine and trains medical students in nearly all of its departments. Post-graduate medical and dental residents are also trained at JMC, although there is no training program for physician anesthesiology.
From March to the end of May, 1255 COVID-19 positive patients were admitted to JMC for care. All in all, JMC saw over 1500 COVID-19 related patient visits. Unfortunately, 319 of the patients seen at the hospital succumbed to Coronavirus. During this time period, our medical staff increased by more than 25%. Staff members including dental health care workers were redeployed to needy areas, 150 inpatient beds were added, and ICU capacity more than doubled.
The Department of Dentistry/OMFS
The Department of Dentistry/OMFS serves the ambulatory and inpatient oral health needs of the underserved population of the Bronx as well as providing resident education to the 53 residents in 5 different CODA-accredited training programs (general practice residency, pediatric dentistry, dental anesthesiology, oral and maxillofacial surgery, and dental public health) and a fellowship in craniofacial orthodontics. Dental staff includes 15 full and part-time attending dentists as well as per diem dentist/attendings who provide resident supervision in each of the divisions. We are staffed by 24 assistants, four nurses, ten clerical staff members and four administrative personnel to provide support for the 23 operatories and four ambulatory surgery suites in the department.
The Response
Beginning in early March, interdepartmental meetings with senior administrative staff were held to identify service needs and to develop a plan for dealing with an ever-increasing patient load. Within dentistry, daily meetings were held beginning in early March to allay fears, provide support and information, and to update everyone on the current state of our knowledge. An original article, If Not Now, When? (NYS Dental Journal March 2020) was distributed to the staff which outlined dental health care workers’ responsibilities during the pandemic. The article highlighted the immediate need to take action during the crisis, reaffirmed the need for personal protection equipment, and encouraged dental health care personnel to provide care to the sick.
The Department of Dentistry offered its support to the hospital, and for the following 3 months, played an integral role in caring for patients at JMC. Of the department’s 99 staff members, twelve were allowed to exercise the Family and Medical Leave Act (FMLA) and remained at home. Two of these staff members were over 75 years of age, and ten had underlying medical or childcare concerns. A small cohort of staff were left in the dental department’s clinics to provide necessary emergency and urgent oral health care, provide tele-dentistry visits, or solicit and collect PPE donations. A large proportion of the attendings, residents, dental hygienists, assistants, and front desk personnel participated and supported the hospital-wide COVID-19 effort to some degree, and nearly without exception performed in an exemplary manner. Department of Dentistry personnel provided basic hospital services including phlebotomy, spotting (supervising donning and doffing of PPE in COVID-19 in-patient units), contact tracing, patient triage, and clerical functions. As appropriate, the dental department personnel also provided the highest-level medical services as part of the medical, surgical, and ICU teams. The first drive-through nasal pharyngeal swab testing for COVID-19 at JMC was performed by OMFS residents. Pediatric dental residents participated in research on developing and experimental COVID-19 therapies (including remdesvir). OMFS residents staffed a general surgery COVID-19 inpatient unit working alongside surgical residents, taking call and managing patients who were admitted but managing relatively well. Other dental residents worked alongside their senior medical colleagues on non-COVID-19 inpatient units to allow for medical personnel redeployment to more urgent areas. While pre-pandemic the dental residents shared maxillofacial trauma responsibilities with other departments, as of March 16 they took it all.
But the most impressive and exemplary contribution was provided by dental anesthesiology (DA) residents as they were called upon to be the primary staff in a step-down ICU for the most critically ill COVID-19 patients at JMC. Patients in the COVID-19 ICU were suffering from acute respiratory distress for which management protocols were — and still are — evolving. Dental anesthesiologists are trained in intubation, ventilator management, placement and management of arterial lines, and preparation of blood specimens necessary to care for these patients. Throughout their assignment, the residents worked alongside and under the supervision of medical and surgical attendings. The attendings had ultimate responsibility for the determination of the patient’s care plan, but the residents managed the unit and routinely performed intubation and resuscitation of intubated COVID-19 infected patients, and also unfortunately witnessed patients die. The DA and OMFS residents completed approximately 300, 12-hour shifts, on ICU and inpatient wards from mid-March to the end of May alongside and in collaboration with their medical colleagues.
Dental anesthesiology residents reflected on their experience:
I was in the unit every single day because I couldn’t afford to lose a moment with the patients. And when I wasn’t there, I was thinking about them, reading about COVID from Italy and China, and dreaming about them, as if I could somehow impact the trajectory of their illness. Alone, I obviously couldn’t. But as a team, we provided consistency in care, which I believe whole heartedly became our key asset. We actually saved people with incredibly poor prognoses and celebrated those who walked out on their own two feet. —TN
I am there for the families. I speak to them whenever they call. I comfort them as best I can as a liaison, ensuring that their loved ones are as comfortable as they can be. The frequent updates, the distressing news that my patient—their loved one—hasn’t survived, all weigh heavily on me every night. But during these unprecedented times, we are supposed to stay strong for our patients and their families. —SE
The need to ensure psychological safety was always a focus and a priority. Emotional support services came to talk to the staff and were made available as part of our Helping Healers Heal, a program provided by the hospital before the days of COVID-19 to help support providers from burnout and secondary trauma. We reassured our staff of the value of their service, and ensured that PPE and supervision were available during the pandemic surge. After the first three or four weeks, most residents and staff members settled into a workflow and were familiar with the patients, allowing for continuity of care.
A staff survey was conducted at the beginning of June to assess the staff’s reaction to the department and hospital response. The results (66/99, response rate = 66.7%) are presented below. Some staff members (13) became infected with COVID-19, although none were intubated or hospitalized. Respondents agreed or strongly agreed that they were fearful of contracting COVID-19 (87%), received the PPE they needed (82.6%), and were proud of the department’s response (82.6%). On the other hand, work still needs to be done when our staff worked in other parts of the hospital, as 39% of respondents felt they were not needed and 19.5% felt they were not treated with respect. While most respondents indicated they were satisfied with the department’s response, others voiced concerns that they were unprepared to face the pandemic and were unnecessarily placed in dangerous situations. In particular, the staff survey response reinforces the need for communication, from the standpoint of sharing information as well as listening to questions and concerns. The more thorough, honest, and straightforward communication, the better. Sharing the vision of hospital leadership and the purpose with our staff members was critical during the most difficult times of the crisis. 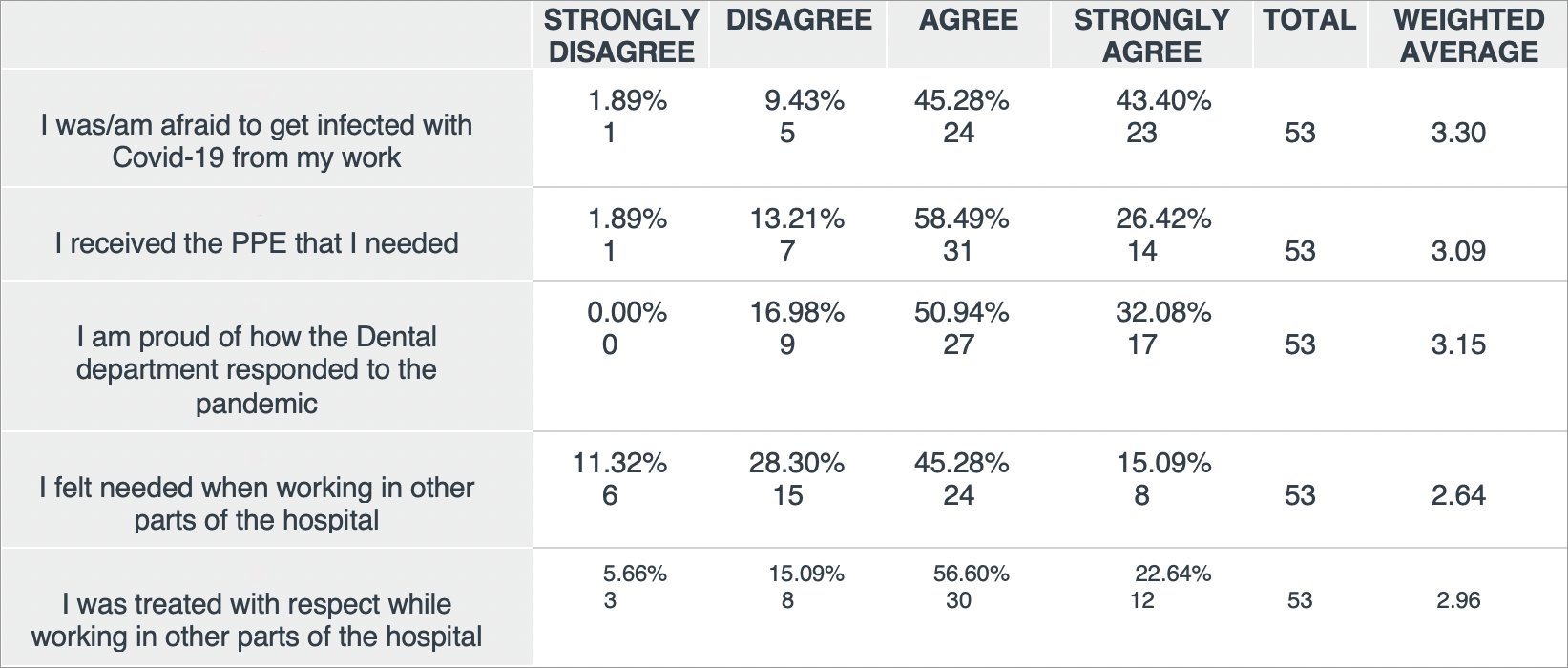
During the month of April 2020, the Department of Dentistry/OMFS provided 361 emergency/urgent dental care visits. This was quite helpful to those in need, however it was an 88% reduction from the number of dental visits provided during prior April 2019. Dental practices were allowed to reopen for routine care on June 1, as long as they adhered to published safety guidelines. Dentists, including those at JMC, newly armed with knowledge on aerosol vs. airborne vs. droplet transmission, viral particle size, room air exchanges, PPE effectiveness, etc. cautiously restarted practicing dentistry according to the “new normal.” The battle is far from over and the dental staff looks forward to resuming regular oral health care. But during these harrowing three months, they exhibited exemplary skill, courage, and bravery as they served admirably alongside their medical colleagues, caring for patients as part of a hospital-wide and national effort to combat the COVID-19 pandemic.
Portions of this article are reproduced from Badner and Saraghi1 with permission of SAGE Journals.
- Badner V. Saraghi M. Using dental health care personnel during a crisis: COVID-19 pandemic in the Bronx, New York. Public Health Rep. 2021;136(2):143-147.
_________
Dr. Victor Badner
Stock photo credits: LeoPatrizi/E+/Getty Images


