Diagnosing COVID-19 in the Dental Office Setting through Observation of Oral Lesions: A Case Report
Dr. Gary Bauman, Dr. Avital Bauman, Dr. Avi Z. Rosenberg
INTRODUCTION
We are now just past the one-year anniversary of the SARS-CoV-2 virus pandemic. Over this time, the spectrum of signs and symptoms of infections have expanded to include findings across many systems, yet there is little that has been reported regarding oral manifestations of the virus. Reports of dentists diagnosing the virus in their patients when they present for routine care are limited. With almost all dental practices closed for routine care for some time, patients avoiding routine care, and dentists diligently pre-screening patients for SARS-CoV-2 infection, it is possible that dentists are simply not seeing patients who have SARS-CoV-2. With the recent dramatic rise in cases including among younger, mostly asymptomatic patients, the potential for dentists to see patients with COVID-19 has increased. As with other viruses, it is the asymptomatic patients that is of the greatest concern of disease transmission to providers and other patients. Thus, identifying these patients and their immediate contacts, will allow for enhanced mitigation.
Reported oral lesions to date in the context of acute SARS-CoV-2 infection include oral vesiculobullous lesions, necrotic oral ulcers and aphthous-like ulcerations early in the course of disease, affecting the tongue, lips, palate, and oropharynx and associated with dysgeusia and vasculocentric lesions.1-3,6,7 Corchuelo and Ulloa presented a case report of an asymptomatic patient infected by her husband who presented with oral lesions4. Sinjari et al in a retrospective study of COVID-19 positive patients reported that xerostomia may be symptom of the virus5. To date, there has been no report of asymptomatic/presymptomatic SARS-CoV-2 infection diagnosis by a dental practitioner on the basis of oral lesions.
CASE REPORT
Two sisters, ages 15 and 17 presented for routine dental maintenance treatment. History on each indicated usually pristine oral conditions with exquisite oral hygiene habits. The 15-year-old sibling exhibited bleeding upon instrumentation and lesions on the gingiva and large lesions on the ventral surface of the tongue were noted (Figure X). Similarly, the 17 year old sibling exhibited bleeding upon instrumentation and leukoplakic aphtous-like lesions were noted on free gingival margins, lip and lateral border of tongue (Figure Y). No other SARS-CoV-2 signs and symptoms were noted at this time. While the 15-year-old patient was unaware of any lesions, her 17-year-old sister attributed these oral lesions to previous history of aphthous ulcers. was vaguely aware of the oral lesions, but disregarded as consistent with aphthous ulcers consistent with past history of similar lesions. Medical and social histories were otherwise non-contributory. Parental consent was obtained to have SARS-CoV-2 PCR testing performed on both patients, a service being offered in our office with a 36-48 hour turnaround.
The patients and first-degree relatives including 44-year-old female, 45-year-old male and 11-year-old female elected to perform SARS-CoV-2 rapid antigen testing (Sofia Quidel) with all but the 17-year-old female testing positive for SARS-CoV-2. These findings were confirmed by PCR testing. Upon subsequent testing, the 17-year-old female seroconverted five days after initial diagnosis. All affected family members immediately commenced a 10-day isolation.
Nasopharyngeal respiratory pathogen panels (adenovirus, influenza A, influenza A H1, influenza A H3, influenza B, Respiratory syncytical virus A, Respiratory syncytical virus B, parainfluenza 1, parainfluenza 2, parainfluenza 3, parainfluenza 4, Coronavirus 229E, Coronavirus OC43, Coronavirus NL63, Coronavirus HKU1, hinovirus/enterovirus, human metapneumovirus, human Bocavirus, Chlamydophila pneumoniae and Mycoplasma pneumoniae) were negative for all.
All cohabitants maintained a daily symptom log. While most family members remained essentially asymptomatic, when presented with a comprehensive list of symptoms, it was clear that they were symptomatic but without the current diagnosis would have attributed these symptoms to any number of other ailments. Some of the mild symptoms included a low-grade fever for a day or two, diarrhea for several days and loss of appetite. The father had the most severe symptoms with longer-duration fever, severe fatigue and insomina. He, as well, developed oral lesions in the floor of the mouth, Some of these symptoms persisted for several days after quarantine ended. Upon follow-up the oral lesions for all patients resolved completely in 7-10 days.
DISCUSSION
There is a great deal not yet understood about the SARS-CoV-2 virus. All health care practitioners need to be aware of the level of asymptomatic transmission in the community and that they are almost surely seeing patients who have asymptomatic disease. Dentists in particular are at risk in that as a respiratory virus, working in the oral cavity is a close encounter with the virus, exacerbated though the performance of aerosolizing procedures. In addition, it is important for dentists and their auxiliaries to be mindful that oral lesions may be a strong indication of asymptomatic COVID-19 disease. When examining patients in the current era, the differential diagnosis of oral lesions should include acute SARS-CoV-2 infection. Patients should be counseled to immediately seek testing and to quarantine until a definitive diagnosis is returned. Dentists can facilitate this process by offering access to testing, both PCR and rapid, in their offices.

Lesions in 15-year-old day of diagnosis

Lesions in 17-year-old day of diagnosis

Lesions in 17-year-old day of diagnosis
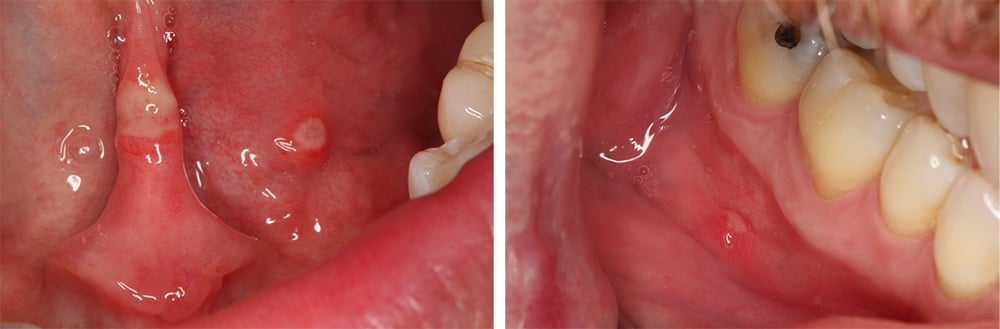
Lesions in 45-year-old father 5 days post diagnosis
__________
Dr. Gary Bauman1, Dr. Avital Bauman2, Dr. Avi Z. Rosenberg3
1 Private Practice, Baltimore Center of Advanced Dentistry, Lutherville, MD
2 Department of Emergency Medicine, University of Rochester Medical Center, Rochester, NY
3 Department of Pathology, Johns Hopkins University School of Medicine Baltimore, MD
- Martin Carreras‐Presas, C., Amaro Sanchez, J., Lopez‐Sanchez, A. F., Jane‐Salas, E., & Somacarrera Perez, M. L. (2020). Oral vesiculobullous lesions associated with SARS‐CoV‐2 infection. Oral Diseases, 1–3. https://doi.org/10.1111/odi.13382
- Thaís Bianca Brandão 1, Luiz Alcino Gueiros 2, Thayanara Silva Melo 2, Ana Carolina Prado-Ribeiro 3, Ana Cristina Froelich Alo Nesrallah 4, Gladys Villas Boas Prado 5, Alan Roger Santos-Silva 6, Cesar Augusto Migliorati 7 Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 Aug 18;S2212-4403(20)31119-6. doi: 10.1016/j.oooo.2020.07.014. Online ahead of print.
- Roberto Onner Cruz Tapia 1, Alberto Jose Peraza Labrador 2, Douglas Magno Guimaraes 3, Luciano Hermios Matos Valdez 4 Spec Care Dentist. 2020 Nov;40(6):555-560. doi: 10.1111/scd.12520. Epub 2020 Sep 3.Oral mucosal lesions in patients with SARS-CoV-2 infection. Report of four cases. Are they a true sign of COVID-19 disease?
- Corchuelo J, Ulloa FC. Oral manifestations in a patient with a history of asymptomatic COVID-19: Case report. Int J Infect Dis. 2020 Nov;100:154-157. doi: 10.1016/j.ijid.2020.08.071. Epub 2020 Sep 1. PMID: 32882435; PMCID: PMC7462545.
- Sinjari B, D'Ardes D, Santilli M, Rexhepi I, D'Addazio G, Di Carlo P, Chiacchiaretta P, Caputi S, Cipollone F. SARS-CoV-2 and Oral Manifestation: An Observational, Human Study. J Clin Med. 2020 Oct 7;9(10):3218. doi: 10.3390/jcm9103218. PMID: 33036482; PMCID: PMC7600761.
- Sinadinos A, Shelswell J. Oral ulceration and blistering in patients with COVID-19. Evid Based Dent. 2020;21(2):49. doi:10.1038/s41432-020-0100-z
- Iranmanesh B, Khalili M, Amiri R, Zartab H, Aflatoonian M. Oral manifestations of COVID-19 disease: A review article [published online ahead of print, 2020 Nov 25]. Dermatol Ther. 2020;e14578. doi:10.1111/dth.14578


