In a retrospective study, researchers found an association between implant failure and patients’ historical use of sertraline, a selective serotonin reuptake inhibitor (SSRI). They published their findings in the March issue of Journal of Prosthodontics.
“When prosthodontic care for tooth loss includes an implant surgical phase, it is important to establish realistic expectations for patients by considering their specific health and medication profiles,” researchers wrote. “The association between implant failure risk and medication use has been investigated by several groups, and conflicting results have been reported regarding the influence of selective serotonin reuptake inhibitors (SSRIs) on implant failure.”
Researchers cited a previous evaluation of patients seen from 1983 through 2014 that showed no significant association between implant failure and SSRI medication use. That analysis, however, pooled various SSRIs rather than estimated the effects for any single medication, an approach that may have confounded results.
Researchers determined that a more detailed understanding of SSRIs and their effects on implants was warranted given the prevalence of the drugs. They used a clinical database design for outcome assessment to identify associations between implant failure and SSRI use in a cohort of consecutive patients seen from 1995 through 2014. In their approach, they assessed patients’ histories of SSRI use, active SSRI use, and SSRI use during follow-up with implant failure. They analyzed SSRIs divided into 6 groups of medications: citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline.
To conduct their study, researchers reviewed the records of 5,456 patients who had a first implant placed at Mayo Clinic in Rochester, Minnesota, from January 1, 1995, through December 31, 2014. Patients had a median age of 53 years. More than one-half of the patients were women (3,143, 58%) who received their first dental implant during the study period. Researchers adjusted all associations for age at first implant, sex, and era of first implant.
Implant failure occurred in 529 patients at a median of 0.5 years. The median duration of follow-up was 5.3 years for the 4,927 patients who did not have implant failure. Analysis revealed that of the 6 SSRI medications, only sertraline was significantly associated with implant failure. As such, sertraline was associated with a 60% greater risk of experiencing implant failure.
“The findings also suggest that use of multiple SSRIs significantly increases risk of implant failure,” researchers wrote. “Compared with patients with no history of SSRI use, patients who used 2 or more SSRIs had significantly greater risk of implant failure.”
Researchers declared that the strengths of their study include its 20-year follow-up period, the size of the cohorts of individual SSRI users and controls, the various temporal relationships investigated, and the robust nature of the electronic health record and prospective database used for data abstraction. They named limitations, too, including weaknesses inherent in retrospective cohort studies and concern that risk analysis estimates applied predictively are best applied to the patients from whom the data were derived, which may limit generalizability of their findings.
Read the original article here or contact the ADA Library & Archives for assistance.
Porous tantalum trabecular metal versus titanium alloy implants
Porous tantalum trabecular metal (TM) dental implants were more favorably osseointegrated with less bone loss than titanium alloy (Ti) implants in a retrospective analysis published in the March issue of The Journal of Prosthetic Dentistry.
“The success of modern dental implants depends on improving bone implant contact or osseointegration,” researchers wrote. “Recently, [porous tantalum trabecular metal] has been incorporated into conventional dental implants. [Porous tantalum trabecular metal]-enhanced titanium alloy implants . . . have shown promising results when immediately loaded and have also been suggested for use in compromised bone and in conjunction with bone regeneration.”
Researchers referenced another retrospective study that demonstrated promising results when using TM dental implants in conjunction with guided bone regeneration for immediate implants. They also pointed to 2015 and 2016 clinical reports proposing use of demineralized bone matrix (DBM) putty in conjunction with implant placement.
They focused their study retrospectively on TM implants compared with Ti implants, analyzing survival rates and clinical bone loss after loading, and on the clinical effects of DBM when used with implant placement. Their hypotheses were that TM implants would exhibit less bone loss after the first year of implant placement compared with Ti implants and would show more bone gain after DBM grafting.
Inclusion criteria for the study needed to be met. They were patients received either TM or Ti implants and had restorations completed from January 2011 through December 2015. Patients had to be at least 18 years old and in good health. Researchers excluded implants with non-DBM bone grafting and those using a barrier membrane.
A single practitioner performed all surgical and prosthodontic procedures and 3 independent investigators reviewed charts. These investigators obtained patient demographic information, including age, sex, race, and ethnicity, and documented implant diameter, length, location, placement type (delayed or immediate), grafting materials (if used), and clinical complications (delayed healing, postoperative pain or discomfort, and prosthetic complications). The investigators measured mesial and distal marginal bone loss from periapical radiographs at each treatment and at recall visits. They determined peri-implant bone levels in conjunction with other clinical outcomes, measuring at the mesial and distal sites of the implant from preoperative and postoperative radiographs. They calculated bone gain and loss and averaged mesial and distal bone levels for analysis, focusing on the first year of placement.
The review spanned 5 years with 82 patients receiving 205 implants (44 TM and 161 Ti implants serving as the control). Key outcomes were that bone grafts were less common in Ti implants (8% versus 32% in TM implants, P < .001) and fewer Ti implants were placed immediately after extraction (12% versus 30% in TM implants, P = .006), no implant was lost in the TM group (100% survival), and 3 implants failed in the Ti group (98% survival). Also, the 122 implants without DBM showed a mean (standard deviation) bone loss of 0.24 (1.09) millimeters, and the 24 implants with DBM had a mean (standard deviation) bone gain of 0.22 (1.27) mm.
Multivariate logistic regression analysis demonstrated that the odds of having bone loss was 64% less in the TM group than in the Ti group after controlling for bone grafting, implant location, immediate placement, bone type, and pretreatment bone level. TM implants exhibited a 0.28-mm bone gain on average, whereas Ti implants had 0.22 mm of marginal bone loss after the first year of loading.
The investigators’ total findings led them to conclude that TM implants exhibit less peri-implant bone loss than do Ti implants. Clinical implications from their study included that TM implants may be appropriate for implant sites requiring bone augmentation and that TM with and without DBM may prevent peri-implant bone loss. In addition, “Demineralized bone matrix may improve bone augmentation regardless of implant types,” researchers said.
Read the original article here or contact the ADA Library & Archives for assistance.
Survival rate of zygomatic implants
Zygomatic implants in patients with severe atrophic and resected maxilla have high survival rates and can predictably support fixed or removable prostheses up to 18 years, according to a retrospective cohort study published in the March/April issue of The International Journal of Oral & Maxillofacial Implants.
“One of the main requirements for implant placement is that there is sufficient bone quality and volume to support an implant retained prosthesis,” researchers wrote.
“Techniques for the placement of zygomatic implants, which engage the zygomatic bone for support, were devised in the early 1990s by Brånemark as an alternative to the placement of shorter implants in patients with a severely resorbed maxilla who could not undergo bone augmentation surgery.”
Although placement of zygomatic implants is challenging owing to difficulty in navigating the complex anatomy during site preparation and the placement of relatively long implants, researchers determined that postoperative complications are infrequent and that these implants can be an attractive option for patients not wanting bone augmentation procedures, which can fail and cause considerable morbidity.
To evaluate survival rates of zygomatic implants, the British researchers designed a retrospective, observational study of anodized and machine surface zygomatic implants placed by 3 practitioners at a primary care setting and a secondary care setting over 18 years. They included patients with a wide spectrum of indications, including extreme bone loss from dentoalveolar and facial trauma; bone loss due to cancer; developmental defects, such as cleft lip and palate; and severe alveolar atrophy due to the loss of natural dentition.
Surgeries evaluated in the study happened from June 1999 through November 2017 at Kingston Hospital National Health Service Foundation Trust (secondary care) and Elmfield House Dental Practice (primary care). Researchers included in the study patients who had zygomatic implants placed to support prostheses after oral cancer, maxillofacial trauma, or unstable removable prostheses or to replace failing dentition. The patients were all treated from 1999 through 2017.
Researchers analyzed 45 patients (42-88 years old) with 88 zygomatic implants, 54 of which were immediately loaded. None of the patients had acute or recurrent sinusitis before implant placement. Patients received either standard or customized zygomatic implants (21 at Kingston Hospital National Health Service Foundation Trust and 24 at Elmfield House Dental Practice). In total, 45 surgeries occurred.
In all, 5 failures occurred across 3 patients for an implant-level cumulative failure rate of 5.68%, leaving an overall implant survival rate of 94.32%.
With the low number of failures, researchers could identify no potential risk factors for failure.
Read the original article here or contact the ADA Library & Archives for assistance.
Virtual 3D modeling benefits dental students, patients
Dental educators can use 3-dimensional (3D) digital design software, available for free online, to develop virtual models of removable partial dentures (RPD) to enhance instruction to both students and patients, according to an article in the April issue of Journal of Prosthodontics.
“Three-dimensional models have been used in dental education and have demonstrated increased spatial visualization by students,” the authors wrote. “However, most of these 3D generating programs are subscription based, or are in their developmental infancy. In addition, they generally do not give the user freedom over what to create or how to deliver the teaching material in a 3D platform or format.”
The authors, from the College of Dentistry at the University of Iowa in Iowa City, Iowa, declared that removable prosthodontics education can be challenging for dental students. “At the University of Iowa, the use of 3D modeling software has enabled the creation of 3D models that can be altered or customized to be used in a more flexible way to teach students in the arts and complexities of removable partial denture design and associated components.”
In their article, they aimed to demonstrate how free online 3D digital design software can be used to manipulate and integrate STL files into 3D models that then could be incorporated into PowerPoint presentations and used to improve understanding about RPD design and components.
The 2 examples of free, Web-based 3D modeling software products available that the authors cited were Meshmixer and Paint 3D.
“Future studies using this 3D educational methodology will evaluate the effectiveness of 3D modeling and virtual design relative to enhanced student learning within the classroom, laboratory, and clinic using the educational 3D techniques described in this article,” the authors wrote.
The article includes links to several videos demonstrating the usefulness of 3D modeling software. The videos demonstrate developmental and educational techniques using the software to create 3D virtual models.
Read the original article and view the videos here or contact the ADA Library & Archives for assistance.
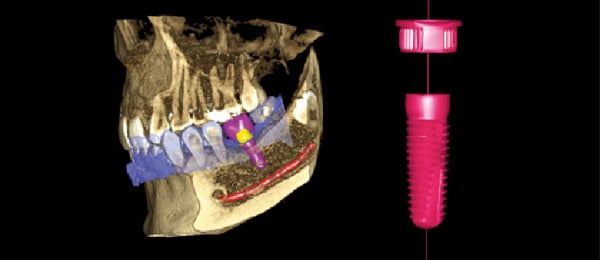
The ultimate virtual implant workflow
Increase confidence and ensure predictable outcomes by utilizing the most advanced digital implant workflow solution available only from Planmeca.
Combine cone-beam computed tomography images, acquired with Planmeca 3D imaging units, together with STL (Standard Tessellation Language, or stereolithography) files from Planmeca Emerald in our Planmeca Romexis software to create restoratively driven implant treatment plans. Then, print your surgical guides in-house with our high-speed Planmeca Creo C5 3D printer. Complete your workflow by milling the final restoration in your office with Planmeca PlanMill 30 S.
Planmeca provides the most complete digital implant workflow, using one software solution for efficiency, integration and success.
Prosthodontics courses at ADA FDI World Dental Congress
The ADA FDI 2019 scientific program offers Prosthodontics courses among the extensive selection of over 350 continuing education courses Sept. 4-8 in San Francisco. Basic registration is FREE for all ADA members and North American attendees. Streamlined pricing makes it easy to find the courses that speak to your personal needs and interests.
Courses to consider:
- Full-Arch Implant Reconstruction: Treatment Planning (#5107), CE Hours: 2.5
- Oral Facial Reconstruction of Complete Nose and Maxilla: A Live Patient Course (#5151), CE Hours: 2.5
- A New Era in Fixed and Removable Prosthesis Attachments: A Hands-On Workshop (#7205), CE Hours: 3
Register today at ADA.org/meeting.
ADA CE Online prosthodontics courses  Need CE? ADA CE Online has hundreds of hours of CE that you can earn from the comfort of your own home. Take a look at our courses focused on prosthodontics that you can implement in your own practice. Too many to choose from? Take them all! Get an ADA CE Online subscription for one year and enjoy unlimited access. Subscribe now.
Need CE? ADA CE Online has hundreds of hours of CE that you can earn from the comfort of your own home. Take a look at our courses focused on prosthodontics that you can implement in your own practice. Too many to choose from? Take them all! Get an ADA CE Online subscription for one year and enjoy unlimited access. Subscribe now.
Upcoming courses for prosthodontists Prosthodontists and office staff are welcome at the inaugural Practice Management Course in Chicago on Saturday, Aug. 10. Speakers will cover marketing, social media, human resources, financial planning, medical billing & coding, and practice transitions.
Prosthodontists and office staff are welcome at the inaugural Practice Management Course in Chicago on Saturday, Aug. 10. Speakers will cover marketing, social media, human resources, financial planning, medical billing & coding, and practice transitions.
The 2019 Prosthodontic Review Course will be held in New York City, Sept. 21-22. Covering the entire spectrum of contemporary prosthodontics, speakers will review core concepts in fixed, removable, and implant prosthodontics as well as an overview of the latest developments in dental materials and digital workflows.
The 49th Annual Session of the American College of Prosthodontists will take place at the Fontainebleau in Miami, Oct. 30-Nov. 2. Under the theme of “Excellence at the Crossroads of Technology and Biology”, speakers will deliver evidence-based presentations on advanced biomaterials and technology, guidelines for tooth preparation, and complex patient care.
For program information or to register, visit Prosthodontics.org or call 312-573-1260.

The consulting editor for JADA+ Specialty Scan — Prosthodontics is Donald A. Curtis, DMD, FACP, Diplomate, American Board of Prosthodontics Professor, University of California San Francisco. |
|