Lebanese researchers found significant differences in efficiency and gingival response among several cordless gingival displacement systems in a controlled clinical trial study. They reported their findings in the February issue of The Journal of Prosthetic Dentistry.
A clean and visible operating field is required in obtaining clinically acceptable impressions that are essential to the success of definitive restorations. Achieving such an environment involves the clinical management of the marginal gingival tissues, crevicular fluids, and localized bleeding.
Mechanical displacement of gingival tissue typically involves a cotton cord placed into the gingival sulcus for temporary tissue displacement. A medicament, most commonly aluminum chloride, is used in combination with displacement cords to temporarily shrink the gingiva by constricting blood vessels.
“Although the conventional chemicomechanical cord technique is widely used, packing the cord into the sulcus may cause pain and bleeding,” researchers wrote. “Other problems include potential damage to junctional epithelium and violation of biological width, which might lead to bone loss and recession or even infection.”
In their study, researchers noted several advantages of cordless displacement techniques over conventional cord techniques, including saving time, less patient discomfort, better gingival displacement, less associated crevicular fluid flow, less application-generated pressure, and better maintenance of gingival health.
Unaware of any other studies that evaluated the clinical efficiency of cordless systems and gingival and periodontal indexes over time, researchers sought to provide an evaluation by comparing some of these systems. Their purpose specifically was to evaluate the effects of 4 cordless displacement systems on the amount of gingival displacement and on the changes in the periodontal tissues, as monitored by recording the plaque index, gingival index, and attachment level.
Their null hypothesis was that there would be no significant differences in efficiency, gingival recession, and gingival health among the 4 cordless gingival displacement systems evaluated in their study.
The controlled clinical trial was conducted at the Department of Oral Rehabilitation clinics, Faculty of Dentistry, Beirut Arab University, Beirut, Lebanon. Researcher included 120 teeth in 30 participants allocated into 4 groups of cordless displacement materials. Participants were 25 through 35 years old. Other inclusion criteria were the presence of first molars; need for complete coverage restoration; abutment teeth of normal size, contour, and position; nonsmoker for at least 6 months before the study; systemically healthy with no medical history that could affect periodontal condition; clinically and radiographically healthy gingiva and periodontium around the abutments; good oral hygiene with pocket depths 3 millimeters or less; no evidence of attachment loss, bleeding on probing, or plaque accumulation; and thick gingival biotype.
To conduct the study, researchers took baseline measurements of periodontal indexes (plaque index and gingival index) and obtained digital scans. They applied the cordless gingival displacement pastes according to the manufacturers’ instructions. They obtained additional digital scans after removing the pastes. On days 2 and 14, researchers recalled the patients to again measure periodontal indexes and obtain digital scans. They compared superimposed screenshots to measure changes in the gingiva. They tested statistical differences among the different materials in achieving lingual and buccal vertical gingival displacement by applying related-samples Friedman 2-way analysis of variance test at 3 intervals (baseline, 2 days, and 14 days) (α = .05).
In both vertical and horizontal gingival displacement, researchers found significant differences among the 4 tested systems. They found that 3 of the 4 exceeded the 200-micrometer requirements for horizontal displacement, while 1 of the 4 provided the least displacement in both vertical and horizontal dimensions.
The researchers declared that clinical implication for their study is that cordless gingival displacement systems are suitable for routine use in restorative dentistry. “They provide the required horizontal displacement for the gingival tissues away from the finish line, making them a suitable alternative to the conventional cord,” researchers wrote. “They can provide hemostasis and preserve gingival and periodontal health.”
Read the original article here or contact the ADA Library & Archives for assistance.
Digital versus conventional laboratory fabrication workflows, time efficiency
Computer-aided design and computer-aided manufacturing (CAD-CAM) work flows produce fabricated zirconia-ceramic posterior fixed partial dentures (FPD) quicker than the conventional lost-wax casting process, Swiss researchers found in a study published in the February issue of The Journal of Prosthetic Dentistry.
Zirconia, which has favorable mechanical properties for use as dental framework material, could not be fabricated as dental prostheses before CAD-CAM technology was introduced in the 1990s, researchers wrote. Now, different CAD-CAM production possibilities exist for zirconia restorations.
“Computerized technology allows laboratory procedures to be performed anywhere in the world, enabling prostheses to be fabricated where production costs are low,” researchers wrote. “However, despite the use of standardized CAD-CAM systems in the laboratories evaluated, a large variability of the framework quality has been reported, leading to increased time spent adjusting the framework.”
Despite these challenges, CAD-CAM technology may save time in the laboratory by reducing some manual labor in conventional fabrication processes, the researchers wrote.
Given that they found a need for clinical studies assessing time efficiency of CAD-CAM laboratory manufacturing processes compared with that of conventional work flows, researchers aimed to evaluate the time efficiency of 3 different CAD-CAM systems and a conventional work flow in fabricating a posterior 3-unit FPD. Their null hypothesis was that the choice of CAD-CAM system or traditional manual work flow would have no effect on the laboratory production time. However, their study results invalidated this statement.
To conduct their study, researchers recruited 10 participants who needed a posterior 3-unit FPD. The researchers set up 3 different digital work flows, including an intraoral digital scanner and the corresponding CAD-CAM system, to evaluate during the fabrication of a posterior 3-unit FPD.
They recorded time for cast fabrication, for the 3-unit framework, and for the veneering process. They also recorded chairside time during the clinical appointment to evaluate the framework. Ultimately, they found that the conventional work flow had a mean working time of 370 minutes, which was significantly higher than that of the CAD-CAM work flow, which had a mean working time ranging from 217 through 262 minutes.
Their study was the second in a series of related investigations comparing digital and conventional work flows for fabricating posterior 3-unit FPD. Part 1 of the series was an investigation into the clinical time efficiency of digital scans compared with conventional impressions. Part 3 (summarized in the following scan) assessed the marginal and internal discrepancy of the digitally and conventionally fabricated frameworks with the replica technique.
The researchers main conclusions included these findings: digital work flow significantly shortened laboratory working time compared with that of the conventional work flow. In addition, centralized manufacturing significantly reduced time efficiency and conventionally fabricated noble alloy frameworks had better marginal integrity than did CAD-CAM fabricated zirconia frameworks. The clinical implications for their study, according to researchers, are that the fabrication of zirconia frameworks for posterior 3-unit FPDs is more time efficient for dental technicians using CAD-CAM systems than the fabrication of a conventional noble alloy framework using the lost-wax technique. However, researchers determined that shipping time may need to be considered for the zirconia framework and CAD-CAM systems involving centralized production facilities.
Read the original article here or contact the ADA Library & Archives for assistance.
Fit of digital versus conventional fabricated fixed partial dentures
Swiss researchers concluded that zirconia-ceramic 3-unit fixed partial dentures (FPD) fabricated using the computer-aided design and computer-aided manufacturing (CAD-CAM) process fit similarly to or better than conventionally fabricated metal FPDs in the shoulder region but not in occlusal regions. The researchers published their findings in the March issue of The Journal of Prosthetic Dentistry.
“An essential aspect of any restorative workflow is the marginal and internal fit of the resulting prosthesis,” researchers wrote. “Poorly fitting margins are associated with a risk of caries through increased plaque accumulation and microleakage. Internal fit can influence the mechanical stability of the ceramic restoration, and an increased internal discrepancy can reduce retention and increase the incidence of ceramic fractures.”
Finding little evidence from clinical studies comparing the fit of digitally fabricated zirconia FPDs to conventionally fabricated metal frameworks, the researchers conducted a randomized controlled clinical trial (RCT) designed to compare the overall performance of 3 digital and 1 conventional work flow for the fabrication of tooth-supported 3-unit FPDs from the impression to restoration delivery.
The blinded RCT’s design centered on within-participant comparison of 3 digital and 1 conventional work flow for fabrication of tooth-supported, 3-unit FPDs. The RCT was conducted at the Clinic of Fixed and Removable Prosthodontics and Dental Material Science, Center of Dental Medicine, University of Zurich, Zurich, Switzerland. Ten participants were included in the study.
Ultimately, digitally fabricated zirconia 3-unit FPD frameworks had a similar or better fit compared with conventionally fabricated metal frameworks in the shoulder region, although in the occlusal regions conventionally fabricated metal FPD frameworks fit more favorably. “Because of the high intrinsic stability of zirconia, the poor occlusal fit of the CAD-CAM zirconia FPDs is probably not clinically relevant,” researchers wrote.
This study was the third in a series of related investigations comparing digital and conventional fabrication of posterior 3-unit FPD. Part 1 of the series addressed clinical time efficiency of digital scans compared with conventional impressions. Part 2 of the series analyzed time effectiveness in the dental technical work flows.
Read the original article here or contact the ADA Library & Archives for assistance.
One abutment-onetime protocol, bone loss
Reporting in the October 2018 issue of Clinical Implant Dentistry and Related Research, Italian and Japanese researchers determined that restoring single implants in the anterior maxilla using a “one abutment/onetime” (OA-OT) protocol supports stable bone levels.
The researchers noted that patients scarcely tolerate bone loss that could dramatically affect the esthetic outcome in the anterior maxilla. They cited research in recent years that focused on outcomes that preserve buccal bone plate and soft tissues, especially in the esthetic zone. Placing the implant shoulder subcrestally to obtain a more comfortable prosthetic emerging profile and improve soft-tissue esthetic results was 1 proposal they found in other investigators’ research.
Unfortunately, with this approach, bacterial colonization of the microgap in the fixture-abutment junction may have caused increased bone loss, they wrote.
Other authors previously proposed use of a subcrestally placed tapered implant with a progressive thread and a rough collar. Still others suggested that soft-tissue thickness is a factor influencing peri-implant marginal bone loss. Alongside implant-abutment morphology, researchers found that prosthetic handling is considered a compromising factor in the stability of the subcrestal biological area.
“To overcome this peri-implant tissue reaction, recently, the connection of the definitive abutment at the time of surgery has been suggested [OA-OT]. The goal of this treatment concept is to eliminate all the possible stresses that occur on the soft tissue,” they wrote.
Finding a lack of studies with longer follow-up in the dental literature, researchers aimed to investigate over 5 years hard-tissue response to OA-OT protocol in the restoration of implants inserted in regenerated postextraction sites in the anterior esthetic area. Their primary outcome was bone level changes measured mesially and distally to the implant platform. The secondary outcome was to investigate if thin or thick biotypes influenced the bone remodeling.
In describing the materials and methodology for their prospective cohort study, researchers did so in terms of treatment involving first and second surgeries and prosthetics procedure, follow-up controls, radiographic analysis, and statistical analysis.
The investigators enrolled 25 patients in the study, but only 22 patients concluded it. The participants were adults at least 18 years old who were seen in a private practice in Rome, Italy, from January 2011 through January 2012. All patients who were seen in the practice who had at least 1 tooth requiring extraction in the maxilla between canines were enrolled.
Researchers performed ridge preservation after extraction. Six months later, they surgically inserted an implant midcrestal and obtained intraoperative impressions. They inserted an immediate definitive abutment with a provisional crown 2 months later.
Researchers obtained periapical radiographs at the final crown connection. They obtained 5 additional radiographs at 12, 24, 36, 48, and 60 months and conducted independent sample t tests to compare bone loss at different times. They based bone loss measures on the average of paired mesial and distal values obtain at the 5 time points.
“The major part of the marginal bone loss took place in the first year and only small bone level alterations could be detected during the subsequent 4-year period of monitoring,” researchers wrote. After 5 years, the mean bone loss was 0.31 millimeters. They used analysis of variance with general linear model to determine any potential role of biotype by comparing thick groups versus thin groups. According to researchers, the analysis of variance showed no statistically significant difference in bone loss among the 2 groups, thin versus thick, over the time (P = .952).
Read the original article here or contact the ADA Library & Archives for assistance.
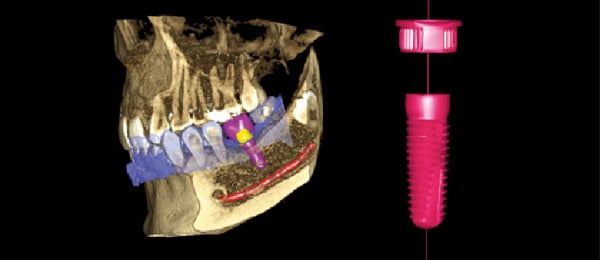
The ultimate virtual implant workflow
Increase confidence and ensure predictable outcomes by utilizing the most advanced digital implant workflow solution available only from Planmeca.
Combine cone-beam computed tomography images, acquired with Planmeca 3D imaging units, together with STL (Standard Tessellation Language, or stereolithography) files from Planmeca Emerald in our Planmeca Romexis software to create restoratively driven implant treatment plans. Then, print your surgical guides in-house with our high-speed Planmeca Creo C5 3D printer. Complete your workflow by milling the final restoration in your office with Planmeca PlanMill 30 S.
Planmeca provides the most complete digital implant workflow, using one software solution for efficiency, integration and success.
Get ready to celebrate National Prosthodontics Awareness Week
National Prosthodontics Awareness Week (NPAW) is April 7-13, 2019. The goal of NPAW is to ensure that patients and dental professionals understand the advanced skills and expertise that prosthodontists bring to patient care.
NPAW events include open houses, public screenings, lunch and learns, press outreach, and more. For media outreach templates and activity ideas, check out the NPAW Toolkit at Prosthodontics.org/NPAW.
Save the date for the ACP Annual Session in Miami, Oct. 30-Nov. 2 The 49th Annual Session of the American College of Prosthodontists will be held in Miami, Oct. 30-Nov. 2.
The 49th Annual Session of the American College of Prosthodontists will be held in Miami, Oct. 30-Nov. 2.
ADA CE Online prosthodontics courses  Need CE? ADA CE Online has hundreds of hours of CE that you can earn from the comfort of your own home. Take a look at our courses focused on prosthodontics that you can implement in your own practice. Too many to choose from? Take them all! Get an ADA CE Online subscription for one year and enjoy unlimited access. Subscribe now.
Need CE? ADA CE Online has hundreds of hours of CE that you can earn from the comfort of your own home. Take a look at our courses focused on prosthodontics that you can implement in your own practice. Too many to choose from? Take them all! Get an ADA CE Online subscription for one year and enjoy unlimited access. Subscribe now.

The consulting editor for JADA+ Specialty Scan — Prosthodontics is Donald A. Curtis, DMD, FACP, Diplomate, American Board of Prosthodontics Professor, University of California San Francisco. |
|