Periodontal status and peri-implantitis
Researchers determined that implant patients with a history of chronic periodontitis, especially patients with severe periodontal disease, had increased risk of developing peri-implant diseases. They published their findings in the August issue of Clinical Oral Implants Research.
Peri-implant diseases, as defined by the World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions, can be divided into 2 categories, peri-implant mucositis and peri-implantitis.
“Peri-implant diseases are a major biological complication of implant therapy, which impair their long-term success,” researchers wrote. “To achieve successful long-term outcomes for implant treatment, peri-implant diseases must be detected and managed earlier to [decrease the potential for] implant loss and reduced patients’ quality of life. Understanding risk indicators and their effect on implant success would help clinicians in preventing implant complications.”
In designing their study, researchers aimed to evaluate the association between factors related to periodontal status and peri-implant diseases to develop an appropriate maintenance protocol. To conduct their study, they evaluated 200 patients with 412 implants. The patients ranged in age from 18 through 79 years, with a mean age of 57.30 years. The cross-sectional study was a survey of the 200 consecutive implant patients in a maintenance program at the Graduate Periodontics clinic in the Faculty of Dentistry at Chulalongkorn University in Bangkok, Thailand, from 1996 through 2014. Each patient had at least 1 dental implant restored with a fixed or removable prosthesis in function for at least 1 year.
Recorded data comprised demographic and implant treatment history, including medical and dental history, periodontal treatment history, and frequency of maintenance care visits, which were all obtained from patient history, chart review, and dental examination. Researchers performed clinical and radiographic examinations during 1 visit and based periodontal care at the implant sites on the CIST, or Cumulative Interceptive Supportive Therapy protocol.
The study details researchers’ approach to clinical examination and radiographic examination, calibration, and statistical analysis. It also includes a section on the case definitions foundational to their work, such as the terms healthy peri-implant, peri-implant mucositis, peri-implantitis, implant survival, past periodontal status, periodontal severity, oral hygiene status, maintenance status, and present periodontal status. The researchers noted that case definitions of peri-implant diseases vary highly between studies. Significantly, then, they defined peri-implant mucositis as bleeding on probing on at least 1 aspect of the implant and peri-implantitis as radiographic bone changes beyond functional remodeling around the implants in addition to inflammation.
They classified implant health status into 2 groups: a non–peri-implantitis group, which included healthy and peri-implant mucositis, and a peri-implantitis group.
“The data analysis revealed that peri-implant health status was significantly associated with past periodontal status, maintenance status, and present periodontal status,” researchers wrote. “In contrast, no association between implant-related variables and peri-implant health status was found in this study.
“We observed a significantly higher prevalence of peri-implantitis (25% vs. 10.9%) in patients with a history of chronic periodontitis compared with those without a history of periodontal disease,” the researchers continued.
They concluded that patients with a history of periodontitis have a 2.5-fold significant increase in risk of developing peri-implantitis, particularly patients with a history of severe periodontal disease. “Therefore, these patients should be treated and well maintained for the periodontal disease before and after implant placement so that successful long-term outcomes of implant treatment can be achieved,” researchers wrote.
Researchers cited some limitations in their study’s methodology, including obtaining demographic data and history of implant treatment from a secondary data source, which has the risk of being incomplete. They also had difficulty in obtaining baseline radiographs for all patients. Finally, they noted participant-level reporting on the results of implant health status, which is more prone to unavoidable selection bias compared with an implant-level analysis.
Read the original article here or contact the ADA Library & Archives for assistance.

Narrow-diameter versus standard-diameter titanium-zirconium implants
A clinical trial study suggests that narrow diameter titanium-zirconium alloy (Ti-Zr) implants are noninferior compared with standard diameter Ti-Zr implants and have less pronounced bone remodeling. Researchers published their findings in May/June issue of The International Journal of Oral & Maxillofacial Implants.
“Despite favorable results following ridge preservation, resorption cannot be completely prevented, and guided bone regeneration ... may still be required before or at the time of implant placement,” researchers wrote. “... Another alternative treatment in cases of insufficient bone available for adequate implant placement includes the use of narrow-diameter implants (NDIs).”
Researchers cited other studies that showed no significant differences in survival and success rates of NDIs compared with standard-diameter implants (SDIs) but declared that there were no published studies that compared the clinical performance of Ti-Zr NDIs and Ti-Zr SDIs, which prompted the development of their own study.
The aim of their study was to test the hypothesis that narrow-diameter Ti-Zr implants are not inferior to standard diameter Ti-Zr implants in regard to bone-level changes and clinical success and survival. The primary outcome was mean crestal bone–level changes measured between implant building and 12 months after loading. Secondary outcomes were implant success, survival, gingival recession, and patient satisfaction.
Researchers designed a multicenter prospective randomized controlled clinical trial with 50 patients who needed a single-tooth replacement in the anterior canine to canine or premolar region of the mandible or maxilla during the 18-month study. Of the initial 50 patients, who were included if the implant site could accommodate a 4.1 mm-diameter implant, 47 completed the study: 23 patients in the NDI (test) group and 24 patients in the SDI (control) group.
Heavy smokers, pregnant women, patients with severe parafunctional habits, and patients who had any contraindication for oral surgical procedures (such as patients with systemic diseases that could affect the bone) were excluded from the study.
Study locations were the University of Texas Health Science Center in San Antonio, Boston University, the University of California at Los Angeles, and the University of Washington in Seattle.
Researchers ultimately found that both the test and control groups had 100% success and survival rates at 12 months after loading. Mean (standard deviation) crestal bone level from implant loading to 12 months after loading around NDIs was –0.27 (0.34) mm, whereas for SDIs the change was significantly higher at –0.48 (0.67) mm (P= .02).
“The success and the survival rates of Ti-Zr NDIs in the present study were 100%, and these implants demonstrated minimal marginal hard and soft tissue changes,” researchers wrote. “The positive results of the present study are encouraging, and if confirmed in the long term and in a larger number of patients, Ti-Zr NDIs would represent a valid treatment option in clinical situations where narrow edentulous ridges are encountered and implants with a reduced diameter are desired.”
Researchers concluded that while the results of their study may not apply to clinical indications with more narrow ridge widths, the findings are encouraging for narrow diameter Ti-Zr implants—including having the potential to avoid the need for bone augmentation—and suggest noninferiority of the narrow versus standard diameter Ti-Zr implant.
Read the original article here or contact the ADA Library & Archives for assistance.

Prosthodontic, patient outcomes for digital versus conventional work flows
In an intraparticipant clinical study, patients and clinicians both preferred esthetic outcomes from a full digital work flow for screw-retained single-implant crowns compared with from a conventional work flow in a measurement and comparison of the 2, although both work flows yielded acceptable clinical fit and delivery of the crowns within 2 appointments. But patients reported higher satisfaction with the digital work flow. These results were published online June 10 in Clinical Oral Implants Research.
Belgian researchers declared that conventional work flows are still considered the reference standard in implant dentistry while pointing out its various limitations, including the need for more work force, time, and potentially cost. They also mentioned issues revolving around patient discomfort related to conventional work flows.
“The new digital technologies are increasingly used in implant dentistry to improve or solve some of the limitations observed with conventional approaches,” researchers wrote. “The combination of intraoral optical scanner (IOS) and computer-aided design/computer-aided manufacturing (CAD/CAM) are nowadays offering the possibility to manufacture monolithic full-contour crowns without any physical model.”
The aim of their clinical study was 2-fold. First, they measured and compared prosthodontic outcomes from preparing a single-implant, screw-retained, monolithic zirconia crown from a conventional work flow with those of a complete digital work flow. Second, they sought to evaluate patient views of the impression procedures and esthetic outcomes of the final crowns as shared through patient-reported outcome measures (PROMs).
Researchers conducted the study according to the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines. They designed their study as a nonrandomized controlled clinical trial with 34 participants, including within-patient comparison of 2 work flows. The participating patients each needed replacement of a single tooth in the posterior maxilla. Inclusion criteria were nonsmoking, in good systemic health, 18 years or older, seeking implant therapy, implant site healed for at least 12 weeks after extraction, presence of an antagonistic tooth, and absence of diastema allowing for the evaluation of at least a mesial contact point.
All patients received a bone-level implant. Thirty of the implants had a regular platform, 3 had a large platform, and 1 had a narrow platform. Each patient was subjected to both a digital and a conventional work flow for the production of 2 screw-retained crowns.
The conventional work flow served as the control while the full-digital work flow was the test.
Researchers measured prosthodontic outcomes on the day of crown placement, evaluating clinical fitting for interproximal adaptation and occlusion. They determined that occlusion and interproximal contacts showed comparable results from the conventional and complete digital work flows (P= .37 and P= .36, respectively).
They obtained PROMS using a visual analog scale (VAS) immediately after each impression procedure at the first appointment and later obtained an esthetic VAS at the second appointment. The clinicians also evaluated esthetic outcomes using the white esthetic score (WES), which was significantly higher in the control group (P< .0001).
“Both the overall WES and VAS scores were significantly better in the conventional than in the digital group,” researchers wrote. “This shows that patients’ and dentists’ opinions were going in the same direction. However, from patients’ opinions, the difference between the two groups was less marked, and most of the patients would also have accepted the experimental crown as a final one.”
Researchers pointed out several limitations for their study, describing most of the measurements as rather subjective, for one. “In addition, the study was neither randomized nor double-blinded; the prosthodontists could easily identify the differences between the two crowns, and therefore, the results have to be interpreted cautiously,” they wrote.
Read the original article here or contact the ADA Library & Archives for assistance.

Keratinized tissue width and peri-implant mucositis
Sufficient width (> 2 millimeters) of keratinized mucosa (KM) may reduce incidence and risk of severity of peri-implant mucositis, German researchers concluded. They published their findings in the May issue of Clinical Oral Implants Research.
A transmucosal region of either masticatory (keratinized) or lining (nonkeratinized) mucosa forms after dental implant placement and abutment connection surgery, the study noted.
“Based on the assumption that a specific amount of KM is necessary to maintain peri-implant health, the transmucosal region of dental implants is either designated as adequate or insufficient,” researchers wrote. “However, the correlation between the width of KM and the prevalence of peri-implant mucositis and peri-implantitis is a matter of an ongoing discussion and recent reviews have been inconclusive on this matter as well.”
The researchers designed a study to test their own hypothesis that a reduced width of KM at dental implant sites is a risk indicator for severity of peri-implant mucositis in periodontally healthy, nonsmoking patients who are highly compliant with maintenance visits.
“The primary objective of the study was to describe the effect of KM on the severity of peri-implant mucositis,” they wrote.
They developed a cross-sectional study and evaluated patients identified within a population of patients with implants receiving maintenance care at the Department of Prosthetic Dentistry and Biomedical Materials Science of Hannover Medical School in Hannover, Germany. The study participants were nonsmoking, periodontally healthy, low-risk patients with at least 1 root-shaped titanium dental implant restored and functioning for at least 12 months who regularly participated (≥ 1/year) in the university’s preventive maintenance program.
Exclusion criteria included had iodine hypersensitivity, had head or neck radiation during the past 6 months, taken bisphosphonates, taken antibiotics during the past 3 months, had a “heart passport,” were smokers or former smokers, were immunocompromised, had diabetes, were pregnant or lactating, had periodontitis, and had metabolic bone disorders.
Researchers examined and evaluated 231 root-shaped dental implants and 52 patients for signs of peri-implant mucositis and the KM width during a 9-month period from January 2015 until October 2015. The researchers clinically measured KM width, plaque index, gingival index, bleeding on probing index, and probing depth.
They analyzed data at the implant level using a generalized estimating equations model, and for sensitivity analysis they used an adjusted linear mixed model. They defined reduced KM as less than 2 mm and 1 mm in width.
Key results were 44 implants in 12 patients who had less than 2 mm of KM and 187 implants in 40 patients who had 2 mm of KM or greater. In nonadjusted analysis of the implant level, reduced keratinized tissue width was significantly associated with peri-implant mucositis (odds ratio 3.3, 95% confidence interval [1.3 to 8.0], P= .009] and severity of disease (mean difference 2.5, 95% confidence interval [0.8 to 4.2] P= .004].
Researchers cited prospective clinical trials that unanimously found that free gingival grafts compared with maintenance alone improved inflammatory parameters in dental implants with insufficient KM. The researchers said that further prospective, randomized clinical trials could determine if augmentation with free gingival grafts, free connective tissue grafts, or xenogene grafts improve peri-implant health and reduce the risk of developing peri-implantitis long term.
Read the original article here or contact the ADA Library & Archives for assistance.
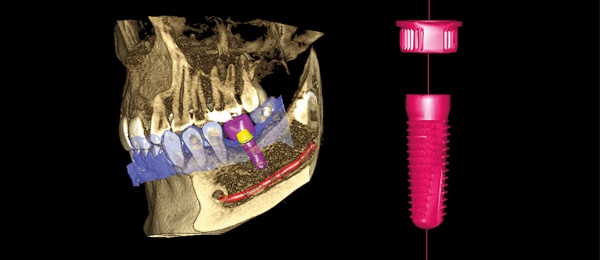
The ultimate virtual implant workflow
Increase confidence and ensure predictable outcomes by utilizing the most advanced digital implant workflow solution available only from Planmeca.
Combine CBCT images, acquired with Planmeca 3D imaging units, together with STL filesfrom Planmeca Emerald in our Planmeca Romexis software to create restoratively driven implant treatment plans. Then, print your surgical guides in-house with our high-speed Planmeca Creo C5 3D printer. Complete your workflow by milling the final restoration in your office withPlanmeca PlanMill 30 S.
Planmeca provides the most complete digital implant workflow, using 1 software solution for efficiency, integration and success.
Get the prosthodontics CE you want at ADA FDI World Dental Congress
 Fulfill your CE requirements and stay informed on the latest developments in the field of prosthodontics Sept. 4-8 in San Francisco. This year’s scientific program offers access to over 400 continuing education courses – including cutting-edge prosthodontics courses.
Fulfill your CE requirements and stay informed on the latest developments in the field of prosthodontics Sept. 4-8 in San Francisco. This year’s scientific program offers access to over 400 continuing education courses – including cutting-edge prosthodontics courses.
Consider the following specialty courses, and more:
- The Missing Link in Implant Prosthodontics (#6137), CE Hours: 2.5
- Managing Technical Complications of Dental Implants (#5121), CE Hours: 1
- Engineered Prosthesis in Guided Implant Placement (#8115), CE Hours: 2.5
Register today at ADA.org/meeting.
What’s causing clinical complications in fixed prosthodontics for your patients?
 Knowledge of the factors that cause complications and failure in fixed prosthodontics enhances your ability to treat and help your patients. Continuing education courses offered by the ADA will help you identify the most common difficulties associated with fixed prosthodontics, as well as methods of minimizing or preventing them. This 5-part series will address various types of fixed prosthodontics and provide the most common issues associated with each.
Knowledge of the factors that cause complications and failure in fixed prosthodontics enhances your ability to treat and help your patients. Continuing education courses offered by the ADA will help you identify the most common difficulties associated with fixed prosthodontics, as well as methods of minimizing or preventing them. This 5-part series will address various types of fixed prosthodontics and provide the most common issues associated with each.
- Clinical Complications in Fixed Prosthodontics: Causes, Prevention, and Management, Part 1
- Clinical Complications in Fixed Prosthodontics: Causes, Prevention, and Management, Part 2
- Clinical Complications in Fixed Prosthodontics: Causes, Prevention, and Management, Part 3
- Clinical Complications in Fixed Prosthodontics: Causes, Prevention, and Management, Part 4
- Clinical Complications in Fixed Prosthodontics: Causes, Prevention, and Management, Part 5
Visit ADACEOnline.org to find out more information about these and other prosthodontics courses.
Upcoming courses in Miami and NYC
The 2019 Prosthodontic Review Course will be held in New York City, Sept. 21-22. Covering the entire spectrum of contemporary prosthodontics, speakers will review core concepts in fixed, removable, and implant prosthodontics as well as an overview of the latest developments in dental materials and digital workflows.
 The 49th Annual Session of the American College of Prosthodontists will take place at the Fontainebleau in Miami, Florida, Oct. 30-Nov. 2. Speakers will deliver evidence-based presentations on advanced biomaterials and technology, guidelines for tooth preparation, and complex patient care. Also included are two hands-on workshops, courses on peer review and media training, and social events throughout the week.
The 49th Annual Session of the American College of Prosthodontists will take place at the Fontainebleau in Miami, Florida, Oct. 30-Nov. 2. Speakers will deliver evidence-based presentations on advanced biomaterials and technology, guidelines for tooth preparation, and complex patient care. Also included are two hands-on workshops, courses on peer review and media training, and social events throughout the week.
For program information or to register, visit Prosthodontics.org or call 312-573-1260.

The consulting editor for JADA+ Specialty Scan — Prosthodontics is Donald A. Curtis, DMD, FACP, Diplomate, American Board of Prosthodontics Professor, University of California San Francisco. |
|